Technical evolution of pediatric neurosurgery: craniosynostosis from 1972 to 2023 and beyond
Federico Di Rocco 1, Mark R Proctor 2
Affiliations expand
- PMID: 37584742
- DOI: 10.1007/s00381-023-06113-w
Erratum in
- Correction: Technical evolution of pediatric neurosurgery: craniosynostosis from 1972 to 2023 and beyond.Di Rocco F, Proctor MR.Childs Nerv Syst. 2023 Oct;39(10):2789. doi: 10.1007/s00381-023-06154-1.PMID: 37715836 No abstract available.
Abstract
Very few clinical entities have undergone so many different treatment approaches over such a short period of time as craniosynostosis. Surgical treatments for this condition have ranged from simple linear craniectomies, accounting for the specific role of cranial sutures in assuring the normal growth of the skull, to more complex cranial vault reconstructions, based on the perceived role of the skull base in affecting the growth of the skull. While a great deal of evolution has occurred, there remains controversy regarding the ideal treatment including the best surgical technique, the optimal age for surgery, and the long-term morphological and neurodevelopmental outcomes. The evolution of the surgical management of craniosynostosis in the last 50 years has been affected by several factors. This includes the awareness of needing to operate on affected children during infancy to achieve the best results, the use of multistage operations, the availability of more sophisticated surgical tools, and improved perioperative care. In some forms of craniosynostosis, the operations can be carried out at a very young age with low morbidity, and with the postoperative use of a molding helmet, springs, or distractors, these operations prove to be as effective as traditional larger cranial reconstructions performed in older children. As a consequence, complex surgical operations have become progressively less utilized. A second relevant advance was the more recent advent of a molecular diagnosis, which allowed us to understand the pathogenesis of some associated malformations and neurodevelopmental issues that were observed in some children despite appropriate surgical treatment. Future research should focus on improving the analysis of longer-term outcomes and understanding the natural history of craniofacial conditions, including what issues persist despite optimal surgical correction. Progress in molecular investigations concerning the normal and pathological development of cranial sutures could be a further significant step in the management of craniosynostosis, possibly favoring a “medical” treatment in the near future. Artificial intelligence will likely have a role in establishing the diagnosis with less reliance on radiographic studies and in assisting with surgical planning. Overall, much progress has been made, but there remains much to do.
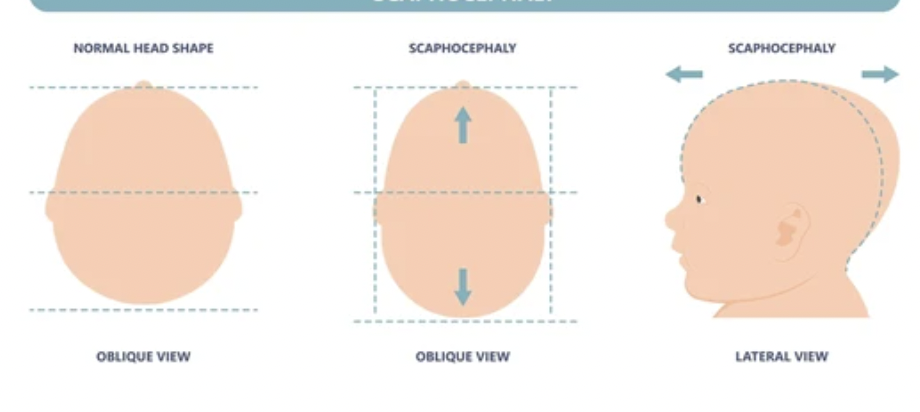
Keywords: Cranial reconstruction; Cranial suture; Craniosynostosis; Endoscopy; Linear craniectomies; Scaphocephaly.
References
- Lannelongue M (1890) De la craniectomie dans la microcephalie. CR Acad Sci 110:1382–1385 https://link.springer.com/article/10.1007/s00381-023-06113-w