In-hospital mortality and length of hospital stay with craniotomy versus craniectomy for acute subdural hemorrhage: a multicenter, propensity score-matched analysis.
Abstract
OBJECTIVE:
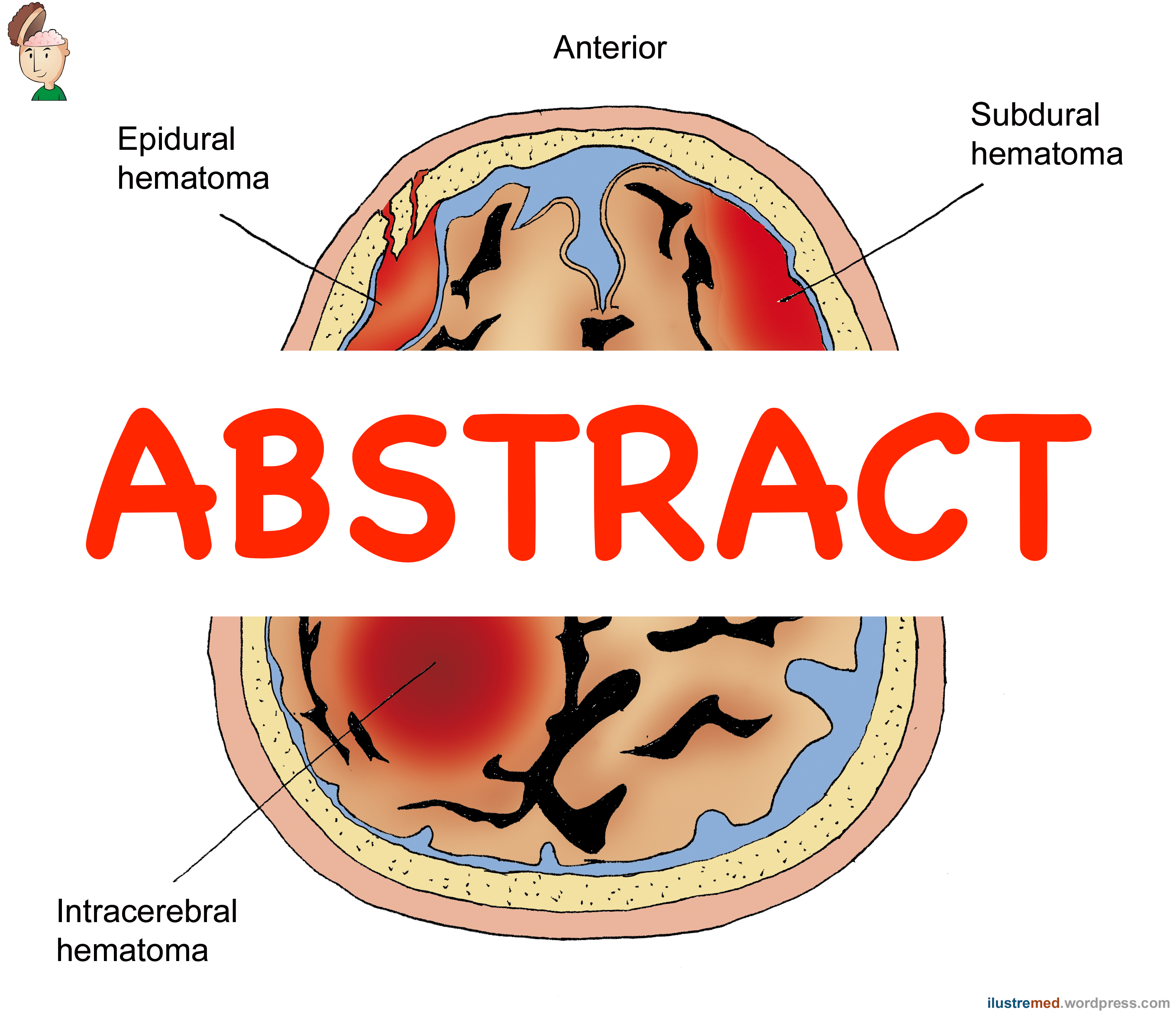
The optimal surgical treatment for acute subdural hemorrhage (ASDH) remains controversial. The purpose of this study was to compare outcomes in patients who underwent craniotomy with those in patients who underwent decompressive craniectomy for the treatment of ASDH.
METHODS:
Using the Japan Trauma Data Bank, a nationwide trauma registry, the authors identified patients aged ? 18 years with ASDH who underwent surgical evacuation after blunt head trauma between 2004 and 2015. Logistic regression analysis was used to estimate a propensity score to predict decompressive craniectomy use. They then used propensity score-matched analysis to compare patients who underwent craniotomy with those who underwent decompressive craniectomy. To identify the potential benefits and disadvantages of decompressive craniectomy among different subgroups, they estimated the interactions between treatment and the subgroups using logistic regression analysis.
RESULTS:
Of 236,698 patients who were registered in the database, 1788 were eligible for propensity score-matched analysis. The final analysis included 514 patients who underwent craniotomy and 514 patients who underwent decompressive craniectomy. The in-hospital mortality did not differ significantly between the groups (41.6% for the craniotomy group vs 39.1% for the decompressive craniectomy group; absolute difference -2.5%; 95% CI -8.5% to 3.5%). The length of hospital stay was significantly longer in patients who underwent decompressive craniectomy (median 23 days [IQR 4-52 days] vs 30 days [IQR 7-60 days], p = 0.005). Subgroup analyses demonstrated qualitative interactions between decompressive craniectomy and the patient subgroups, suggesting that patients who were more severely injured (Glasgow Coma Scale score < 9 and probability of survival < 0.64) and those involved in high-energy injuries may be good candidates for decompressive craniectomy.
CONCLUSIONS:
The results of this study showed that overall, decompressive craniectomy did not appear to be superior to craniotomy in ASDH treatment in terms of in-hospital mortality. In contrast, there were significant differences in the effectiveness of decompressive craniectomy between the subgroups. Thus, future studies should prioritize the identification of a subset of patients who will possibly benefit from the performance of each of the procedures.
KEYWORDS:
AIS = Abbreviated Injury Scale; ASDH = acute subdural hemorrhage; CI = confidence interval; GCS = Glasgow Coma Scale; IQR = interquartile range; ISS = Injury Severity Score; JTDB = Japan Trauma Data Bank; TBI = traumatic brain injury; TRISS = Trauma and Injury Severity Score; acute subdural hemorrhage; craniectomy; craniotomy; mortality; propensity score matching; trauma; traumatic brain injury
- PMID:
- 31226690
- DOI:
- 10.3171/2019.4.JNS182660