Differences in neurosurgical treatment of intracerebral haemorrhage: a nation-wide observational study of 578 consecutive patients.
Abstract
BACKGROUND:
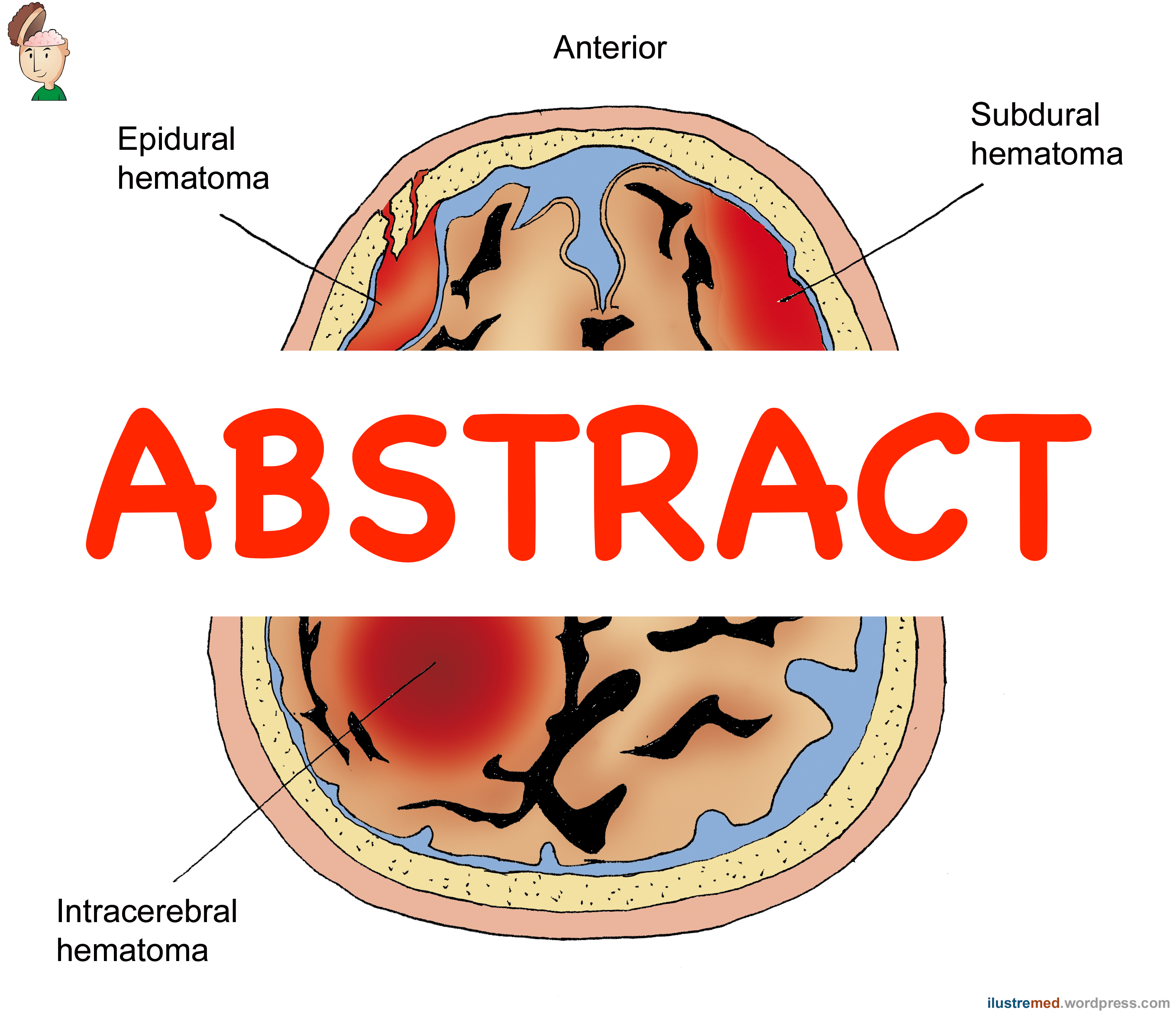
Supratentorial intracerebral haemorrhage (ICH) carries an excessive mortality and morbidity. Although surgical ICH treatment can be life-saving, the indications for surgery in larger cohorts of ICH patients are controversial and not well defined. We hypothesised that surgical indications vary substantially among neurosurgical centres in Sweden.
OBJECTIVE:
In this nation-wide retrospective observational study, differences in treatment strategies among all neurosurgical departments in Sweden were evaluated.
METHODS:
Patient records, neuroimaging and clinical outcome focused on 30-day mortality were collected on each operated ICH patient treated at any of the six neurosurgical centres in Sweden from 1 January 2011 to 31 December 2015.
RESULTS:
In total, 578 consecutive surgically treated ICH patients were evaluated. There was a similar incidence of surgical treatment among different neurosurgical catchment areas. Patient selection for surgery was similar among the centres in terms of patient age, pre-operative level of consciousness and co-morbidities, but differed in ICH volume, proportion of deep-seated vs. lobar ICH and pre-operative signs of herniation (p?<?.05). Post-operative patient management strategies, including the use of ICP-monitoring, CSF-drainage and mechanical ventilation, varied among centres (p?<?.05). The 30-day mortality ranged between 10 and 28%.
CONCLUSIONS:
Although indications for surgical treatment of ICH in the six Swedish neurosurgical centres were homogenous with regard to age and pre-operative level of consciousness, important differences in ICH volume, proportion of deep-seated haemorrhages and pre-operative signs of herniation were observed, and there was a substantial variability in post-operative management. The present results reflect the need for refined evidence-based guidelines for surgical management of ICH.
KEYWORDS:
Craniotomy; External ventricular drain; Guidelines; Intracerebral haemorrhage; Intraventricular haemorrhage; Surgery
- PMID:
- 30877470
- DOI:
- 10.1007/s00701-019-03853-0