Surgical management of acute subdural hematoma: a comparison between decompressive craniectomy and craniotomy on patients treated from 2010 to the present in a single center.
Abstract
BACKGROUND:
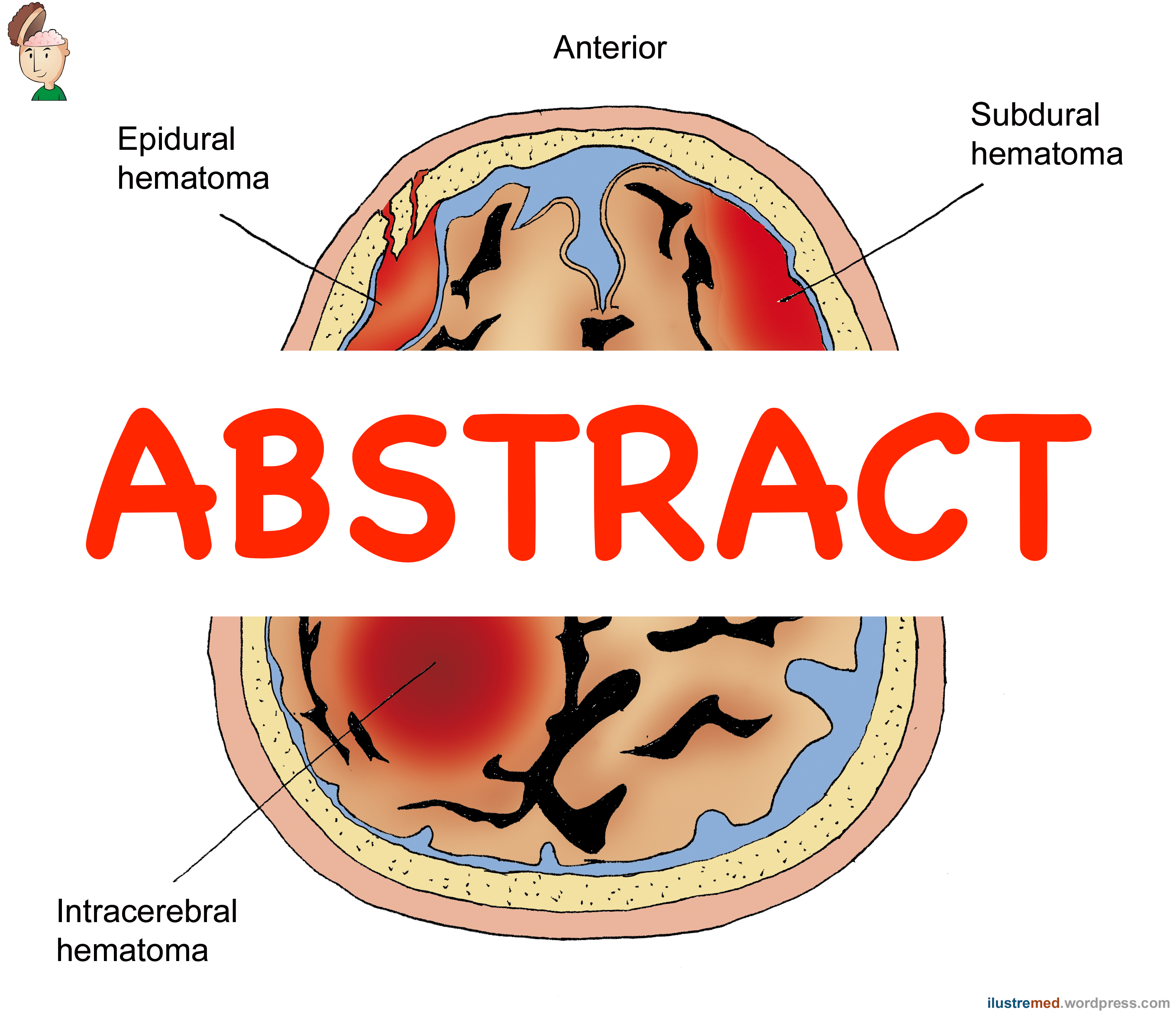
Acute subdural hematoma represents an important cause of disability and mortality. Its surgical treatment takes advantage of two surgical procedures: craniotomy and decompressive craniectomy, nevertheless the effectiveness of one procedure rather than the other is still debated. This study was conducted to identify which of the surgical procedures could provide better neurological outcome after traumatic acute subdural hematoma; as a secondary endpoint, the study tries to settle pre-operative prognostic factors useful to identify the most appropriate surgical technique for every specific patient and kind of trauma.
METHODS:
A retrospective analysis was performed on patients who underwent craniotomy or decompressive craniectomy between January 2010 and July 2017 at the Department of Neurosurgery of Umberto I Hospital in Rome. Ninty-four patients were selected and reviewing clinical records, pre-operative and post-operative’s data were collected (e.g. GCS, mechanism of trauma, CT findings, mortality rate, neurological outcome at discharge, mRS at 12 months). Data were analyzed using X2 test and the F test. The multivariate analysis was performed using a stepwise logistic regression. The analysis was carried out using SPSS software and a p value ? 0.05 was considered significant.
RESULTS:
On 94 patients 46.8% underwent decompressive craniectomy and 53.2% underwent craniotomy. The mortality rate was (53.2%); it was shown to be related to a GCS < 8 (p = 0.033) and to age > 60 years old (p = 0.0001). Decompressive craniectomy was performed most frequently for high energy trauma (p =0.006); the mean GCS at admission was 7.91 for decompressive craniectomy and 9.64 for craniotomy (p = 0.05). Patients who underwent decompressive craniectomy and survived surgery showed a better neurological outcome compared to those who underwent craniotomy (p = 0.009). The evaluation of mRS after 12 months didn’t show a statistically significant difference between the two groups.
CONCLUSIONS:
In case of high energy trauma and GCS ?8 different neurosurgeons decided to perform most frequently decompressive craniectomy rather than craniotomy. Furthermore, even if not related to survival rate, decompressive craniectomy showed a better neurological outcome especially in patients with GCS ?8 at admission. In conclusion, even if prospective studies are required, these results depict the current attitude about the choice between craniotomy and decompressive craniectomy.
- PMID:
- 30259718
- DOI:
- 10.23736/S0390-5616.18.04502-2