Fashionable Biotech Exec, MD
Biotech Exec – kicking cancers a$$ with my husband at the family biotech biz; a fashionista, patient, MD (former neurosurg), and blogger www.fashionsurgeon.com
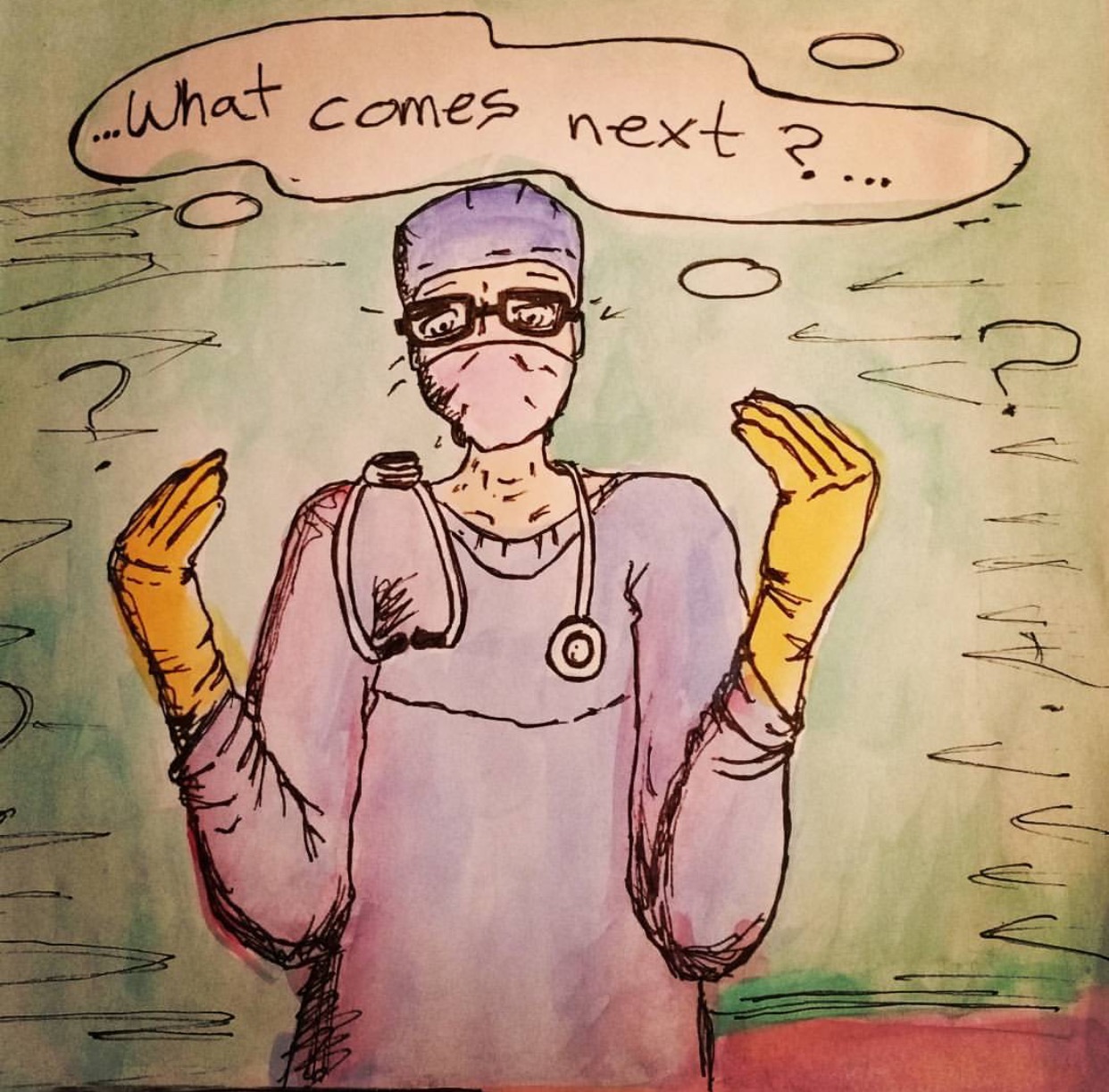
Art by Kathryn Ko @doc_ambidexter on IG
Many people discuss the “Malignancy” of Neurosurgery Residency Programs. There are the stories and legends passed down through generations of residents. The Neurosurgeon who wielded a gun in the OR, or who threw surgical instruments at their assistant. Many of my followers DM me on instagram – “Is it true?.” But it was this Instagram post (that was sent to me by a follower) that inspired me to write about this issue. The following was posted by anonymous @humansofny:
“There’s a strange culture in medicine. People are less friendly to each other than I imagined. I got an MD and PhD in neuroscience. Im finishing my residency right now. I guess I thought that everyone would be compassionate, and would help each other, and would be nice to each other. And don’t get me wrong – I work with with a lot of compassionate people. But the stress just erodes people. There’s a lot of tension and anger. We’re taught that 80 hours per week is normal and shouldn’t be questioned. But at the same time, a huge amount of work that medical interns do is administrative. It could be outsourced without affecting the quality of education or care. And the culture does real harm. I’ve had two friends commit suicide. One of them was studying anesthesiology at Yale and overdosed in a parking lot. The other jumped off the dorm building at NYU. There’s got to be a better way. I don’t know, maybe I’m just saying this because I’m stressed. I’m heading to the ER now. I’m almost at the end of my residency. I can see the end of the tunnel. But the tunnel is very damaging.”
This quote, struck a cord with me, and quickly brought back disturbing memories of my own neurosurgical residency and the dysfunctional, malignant organization of my peers and educators. Now out of residency, I would never tolerate that type of work environment or abuse, but for some reason there are different standards inside the microcosm that is the hospital. But why?
I guess you can track it back to the days of Harvey Cushing, when the term “resident” meant you lived at the hospital. So began the cycle of hierarchal “hazing” that has become the culture of many neurosurgery programs in the United States. And this “culture does real harm,” as quoted above. Not only to the residents, but to the patients. And many Neurosurgeons hold their being a total ass on a power trip in the utmost esteem. Like they should be given a medal for keeping it “like the old days.” Congratulations you taught me nothing, humiliated me and made me envious of those who worked at the hospital McDonald’s, because I doubted those workers went to bed anxious everynight and fearful of what the next day could bring.
Don’t get me wrong their are so many good experiences. The bonds I made with patients and families. The occasional resident who took me under his/her wing and actually took time to teach me. The exhilaration of mastering an operative technique. But the balance needs to tip more this way.
For those of you reading this who are not in medicine or not yet, you may be wondering what the culture was like, and now thinking I was flogged if I didn’t get my attending (fully trained staff neurosurgeon) his coffee on time and the way he liked it. Let me describe some examples.
In my experience, and that of many others, being in neurosurgery residency is very similar to being in a fraternity. In essence you are a slave your PGY-1 and 2 years (like being a pledge) and your life gets easier as you climb the ladder. By your Chief year, you are sitting in the call room watching sports between cases (unfortunately my PGY-2 year was the World Cup), and you do not participate in any other patient care unless an emergency occurs and you usually simply dictate orders. I went to a program which matriculated 3 residents per year. Because of this we had 3 Chief Residents who led each team of approximately 5 other residents (remember some residents are on their research year etc) and approximately cared for 30 patients. The PGY-1 and 2 typically stayed on the floor, wrote all the notes, worked with case management, put out fires and discharged patients (refer to my last blog on “the day in the life of a neurosurgery resident.”). On most every day the PGY-3,4 and Chief had time to help with the floor work, but they did not, because hey they already were the low man on the totem pole and it was their time to relax. This extreme lack of team work ending up putting such a strain on the junior residents that not all of the work was finished at 7pm “hand off time,” to the night float. This would lead to yelling, cussing and eventually the senior residents leaving, letting the junior residents clean up the rest of the work and get home by 9:30pm on a good day.
Lack of team work was one thing but the attitude and poor bedside manner of many neurosurgery residents’ was appalling. There is never a need to wake a floor patient POD #1 from a hemilaminectomy by sternal rub at 5:15 am. Furthermore, the “sink or swim” attitude of many programs is ridiculous when patients’ lives are at stake. Many times I was put into positions, doing procedures with other unqualified junior residents that made me very uncomfortable. I always thought – if this was my family member, shit! But education was often put no the back burner for the Chief to watch a soccer match, and the Attendings whose ultimate responsibility it was to teach us wanted to be called during the critical parts of the operation and then leave, letting the Senior Resident open and close. If you were lucky and second assist you might get to close – but then “you are to slow,” and you take over knot tying and cutting. The worst quality I saw in some of my co-residents was their lack of empathy toward patients. I will never forget when a PGY-3 avulsed a nerve root during a spine procedure and the team thought it was hysterical that he would likely never be able to take a normal piss again. Add in a little sexual harassment (the field being 7% female during my residency) like “hey I hear your fucking Dr. XX,” – all because I took good care of his patients, he noticed and would let me assist in some of his cases as a PGY-1, leaving a PGY-3 out on the floor.
I realize that this is an n =1, and many other programs may be different, but from having colleagues who went to other programs and word of mouth this is way too common of a phenomenon. I lived in fear that first year. I was consistently sleep deprived, and depressed. After a 46 hour call shift, I fell asleep at the wheel and thank god only got in a minor fender bender. And the nights that I could sleep, I was so anxious about my patients, knowing we were not caring for them as well as we should that I tossed and turned.
Recently on one of my instagram posts someone asked me, “Do we have to accept this culture, or do you think it will change?” There are three ways I think the neurosurgical community could dramatically change the culture.
#1: It starts with you, with each individual. Stop the cycle. Just because you “paid your dues,” doesn’t mean you get to check out from your responsibilities of hands on patient care, and educating your junior residents. If one class of residents did this at your program, the next senior residents would…and neurosurgery departments could work as a well oiled machine. Like Yoda up there says, “you must unlearn what you have learned.”
#2 With advances in technology and more operative cases, medicare, Obama care, the patient load is too great. I would suggest PGY-1 year be a general neurosurgical year where you learn not only how to take care of patients on the floor, but you are exposed to the basic neurosurgical procedures (burr holes, decompressive crani’s for trauma cases, etc). And throughout the year you rotate through the neurosurgical subspecialties – spine, functional, cerebrovascular…. By your PGY-2 year I think they should separate cranial and spine surgery into 2 different programs. The techniques are very different as well as the anatomy and pathologies. I think this would improve the resident:patient ratio, and most residents come into their PGY-1 year with some preference.
#3 Neurosurgery departments should hire and utilize PA’s to unburden the junior residents. Even the passionate resident can quickly become jaded after monotonous paperwork and 100 discharge summaries to catch up on your one day off. Barrow’s Neurological Institute (BNI) is an excellent example of utilization of physician assistants. Most days the PGY-1’s operate.
I know some how things can change. I met Dr. Julio Pereira, MD through instagram (of course). His residents and colleagues seem to work extremely well together. And this is in Brazil, where they do not have the technology we have or portable CT scanners in every Neuro ICU. He takes great pride in educating his students and others. So perhaps in the US neurosurgery selects for certain personalities and individuals who are more power and financially driven?
Sorry medical students and premeds with your heart set on neurosurgery – this is not to scare you. It is to be honest and to let you know that 1) program selection is important (sometimes its hard to tell, in my case they were good actors) and 2) Remember you don’t have to assimilate to the culture, you can be the one to help make the change!
Fashionable Biotech Exec, MD
Biotech Exec – kicking cancers a$$ with my husband at the family biotech biz; a fashionista, patient, MD (former neurosurg), and blogger www.fashionsurgeon.com